We are blessed with a community of incredible mother’s who are athletes and athletes who are mother’s, and their information is valuable. We were recently poised with the question – How do I prepare for a marathon when I’m breastfeeding? We encourage those who have experience to use this as a platform in sharing their own stories and advice. The topic of proper fueling as a new mother will be one in a series of topics that will hopefully enhance all of our understanding of the female reproductive athlete as well as celebrate them for their multi-layered accomplishments. In a question/answer series, here is what we’ve garnered:
Q: Can or should you run while breastfeeding?
A: Yes you can – the should depends on you. There is a lot of information out there about how breastfeeding is completely safe for the mother and baby if you’re exercising, but there’s not a lot of information out there about just how much is ok, and at what level of competing is ok. Breastfeeding is not for everyone, but if you decide to breastfeed and want to continue running and racing, it is possible. It might not be easy, especially in the earliest stages, or if your baby is completely dependent on you for nutrition. You alone have to find what works best for you.
A concern of some regarding nursing is the role it plays in bone health. Research shows that 200mg calcium/day from the mother goes into her breast milk, and that this can cause some loss of bone mass at some sites, temporarily, as long as nursing continues. This transfer changes back to normal once nursing is done. Studies show that a baby’s milk calcium composition is not changed by the mother’s calcium intake or lack thereof, meaning that the baby will take the mother’s calcium if there’s not enough to go around. One thing you should keep in mind, is if you’re amenorrheaic (infrequent periods), combined with deficient in calcium, you may suffer from a decrease in bone mass density. If you have a history of stress fractures already pre-pregnancy, you might be at a higher risk for developing them while nursing and training. A bad combo would include: decreased calcium/caloric intake, over-training and abnormal menstrual cycle. Suggestions: Take your prenatal vitamins as instructed by your physician, and continue them through nursing. Consult your MD to discuss if more calcium or Vitamin D is needed.
For some postpartum moms who suffer from depression, running can help. An avid runner, mom and coach, Dr. Kristina Pinto EdD, a specialist in women’s health and psychology, experienced the positive impact running had as she endured her own challenging bout of postpartum depression before rediscovering running. She co-authored the book, Fit and Healthy Pregnancy: How to Stay Strong and in Shape for You and Your Baby, to help athletes adjust to pregnancy and life as a parent. From the book she offers 5 tips to get back in your fitness groove:
- Rest and recover – Pay attention to how your body is healing.
- Set a schedule – This can help you feel more in control of your life.
- Go easy on yourself – Your focus should be on feelinggood, sleeping, taking care of yourself. Don’t rush to lose weight or tackle certain workouts. Throw concrete goals out the window for now.
- Bring baby with you – With ligaments and joints being loose and the potential for your equilibrium to be off, running with a baby jogger can provide the added benefit of support and balance.
- Register! – Pick a few events and put them on the calendar. Even if it’s volunteering. The more accountable you are to the goal, the better. Select a range of goals from ambitious to simple and include ones that aren’t just about speed or distance.
Q: What can I expect?
A: The first few months are considered the hardest. If you can get through them, the rest will come easier. Once you do begin to run, it’s okay if all you can get in is an extremely short run – a few minutes, a few miles – try to restructure the mentality that if the effort is too small or too short, it’s not worth doing. For a while your runs will be determined based on your baby’s schedule and needs, so you’ll have to be flexible with your own. A simple tip – Dress for your run, even if you’re about to nurse, so there’s less intermittent time to change your mind – if you’re ready to head out the door, you have less of an excuse not to. Also know when it’s a better decision to take a nap instead. Be open-minded about breastfeeding’s demand on your body. You might feel okay, but hard training might impact your supply.
Consider researching Glucosamine for your joints if you have achy knees. Postpartum mothers sometimes suffer from achy knees due to the relaxin hormone left in the body, which came about to loosen your ligaments so that the baby could pass through your pelvis. This hormone will stay in your body until you stop nursing. Glucosamine can help and is safe for nursing mothers. As always, consider this with your physician.
Hydrate often. More than. Hydrate Well. Breast milk is made up mostly of water, so you need enough in your body in order to produce enough milk. Try and drink water each time you nurse. As a runner you will need to be even more conscientious. On average, nursing moms drink about a liter more than non-nursing women a day. If anything, a good rule is – Drink to Thirst.
Q: How do I work around pumping?
A: If you are creating enough supply, it’s a good idea to pump an extra bag or bottle a day in the first month or two postpartum. You can freeze them, which will give you freedom to leave for runs later on, or in case you need to travel to races. Once you have a supply built up, you can slow it down, and rotate out the older milk in order to make sure none of your work spoils. Some find pumping a pain, but if you can get through it, you can prepare for small freedoms later on. Mothers generally produce the most milk in the middle of the night, so if you run early in the morning, try to pump or breastfeed before you leave. Your baby will be fed (peace of mind) and you will feel better physically from not waiting so long between nursings.
Q: How can I get creative with my training to ensure it doesn’t affect my nursing or pumping schedule?
A: Run on a treadmill, in loops close to home, or with a jog stroller. For most nursing mothers, the hardest part is being away from the baby. You might feel guilty leaving them to run. But, I think it’s important to take some time away, and to take care of you. It might be hard to convince yourself of this, so to alleviate some of that guilt, run on a treadmill, around your home, or take your baby with you. The sacrifice is that you won’t travel to run “destination runs,” or make it out for a several hour long run, but it’s about finding balance and compromising.
For some, running at about 80% of your previously normal training volume, with no real hard workouts for the first few months is possible. By 6-9 months, after your baby is introduced to solid foods, you might be better set up to fully dive into training. This isn’t always the case, especially if you’ve had multiple pregnancies close together, as there could be a cumulative effect. Again, how much you can do is determinant of your individual story and situation.
Q: What’s the latest TSA rules regarding breast pumps/milk and security?
A: You might have to go through extra screening with TSA, but as I’ve found lately, it’s a toss what you’ll be pulled aside for, and full bottles of toothpaste seem to go through without a hiccup these days. The latest TSA requirements for Formula, Breast Milk and Juice relay that all said items are permitted through security checkpoint, including pumps, but that you will need to separate formula, breast milk and juice from other liquids, gels and aerosols limited to 3.4 oz or 1oo milliliters. TSA officers may test liquids for explosives or concealed prohibited items. If officers are unable to use XRAY to clear these items, they may ask to open the container and have you transfer the liquid to a separate empty container or dispose of a small quantity. Inform TSA if you do not want the formula or breast milk to be XRAY’d or opened, upon which additional steps will be taken to clear the liquid/s, i.e. your travelling partner might have to undergo additional screening procedures, etc. Ice packs, freezer packs, frozen gel packs & other accessories required to cool formula or breast milk are allowed in your carry-on. They are subject to the same screening above. You may also bring gel or liquid-filled teethers, canned, jarred and processed baby food in your carry-on. They request that you only bring as much as will get you through the flight, if possible.
Q: How can I keep my girls in check?
A: Some moms go for 2x sports bras. Brands like CAKE are designed to be supportive & nice-looking with easy snap feeding clips. There’s the Moving Comfort Fiona bra, which is also a nursing-capable sports bra with velcro adjusters to add extra support or let the girls out. Some swear by the brand Bravissimo for their shock absorbing design, ENELL, the Tata Tamer by Lululemon, Nike, Champion Double Dry Seamless. Sports bras can get expensive, especially when you need more technology, support, shock absorption – Check out Amazon for better deals. Dark colors, added breast pads or padded sports bras are good in case of leaking.
Q: Can I pump right before the race? During? When should I after?
A: Your base level goal should be to pump. Even if you have to pump and dump. You can take a pump and for more privacy, a poncho or throw-away blanket to the start line (Note: you will need to plan what to do with the pump if you take it to the start, once finished. A better idea is to leave one in your checked bag at the finish line). Your needs will be determined by how old your infant is and how established your milk supply is. If you’re at the end of nursing, you can usually go longer between pumps, but if you’re only a couple months in, you might need to pump 3-4 hours between, and if you’re running a marathon finishing time of 3-5 hours, it could get uncomfortable. Some women have reported pumping during the marathon, their husbands at a meeting point to grab the goods, or have left a pump and battery pack in their drop bags or with a loved one waiting at the finish line. All of these factors – how established your supply is, what your baby’s schedule is, how long you take to finish – are exclusive to you, and have to be tailored to your routine.
Consider investing in a manual pump – they can go anywhere and do not require batteries or an outlet, and are compact. Perfect for pre-race or to travel with. A manual will cut all the guesswork or lack of control in situations otherwise undetermined.
Q: What about the “Booby Bonk?“
A: From SaltyRunning.com, in an article entitled, Got Milk? Running and Breastfeeding, the notion of the “booby bonk” is questioned regarding running out of glycogen to burn and the nursing mom’s body’s ability to burn fat for fuel to the extent necessary to train for and race a marathon (speculation). In training, racing and breastfeeding you need to take in plenty of calories to successfully tackle proper export and utilization. One of the great things about breast milk is that it can meet your baby’s nutritional needs even when you don’t eat perfectly. But, if you’re too low in calories or eat a disproportionate diet which excludes some necessary nutrients, the quality and quantity of your milk can be affected. When you don’t get the nutrients you need from your diet, your body will draw on its reserves, which leads to depletion. Just as if you were solely training, eating a mix of carbohydrates, protein, and fat at meals will help to keep you feeling full longer and supply your body with the nutrients it needs. Complex carbs like whole grains, cereals, fresh fruits and vegetables not only provide more nutrition than starches and sugars, but will provide longer-lasting energy. When it comes to fat, think mono- and polyunsaturated, like canola oil, olive oil, fatty fish like salmon, avocados, olives, nuts and seeds. Stock up on all these items, make sure you’re peeing light yellow to clear and you’ll find yourself far from booby bonk.
A good rule of thumb is to take in 200-500 calories in excess of what you needed to maintain your weight before you were pregnant, while you are nursing. You use of calories when you nurse. Your body stores up fat during your pregnancy to provide the extra calories needed for milk production. “Eat to hunger.”
Q: Yeah, ok, but what about caloric input during the race?
A: Again, from SaltyRunning.com, in an article called, Fight the Bonk Part II: Pepper’s Magic Marathon Nutrition Formula, Pepper mentions, “I found it hard to believe that everyone’s consumption would be the same, and while the general recommendation of a gel every 30-45 minutes seems a good baseline, I think it generally causes people to overconsume gels and thus get into GI distress territory.” I agree with this, in the way that it’s hard to make an umbrella-consensus regarding proper nutrition, especially if you tack on that you’re breastfeeding/pumping/a new mom in general. Though she offers the following equation, you have to figure out what works for your body, so practice before your race in runs, trying out goos or solid foods and liquids to see what your body accepts and seems to utilize well. This is her proposed marathon nutrient needs calculation:
Weight x .63 x GMP x .3 – Amount of Calories to Consume per Hour of the Marathon
Step 1 – What is your weight in lb’s? Plug this into Weight
Step 2 – The .63 is used to determine how many calories you burn per mile of running. Multiply your weight x .63 and this will tell you approx. how many calories you’ll burn per mile.
Step 3 – GMP = Goal Marathon Pace, in miles per hour. Here is a calculator for converting your pace to miles per hour.
Step 4 – When you multiply the first three steps together, you get the amount of calories you burn per hour, but when you’re running you can only replace/digest at most 30% of those calories. So now we need to take 30% of our calories burned per hour and this is our target calorie intake per hour of the marathon!
Remember that gels don’t kick in for at least 30 minutes; plan when to take your last gel. If you take Gatorade at certain stations, estimate how many calories this would allot you, give or take.
Q: What should I expect post-race?
A: Extra stress on the body will likely dip into your supply. Don’t be discouraged if milk supply seems a little slow for a day or a few days post marathon or hard effort as you’re recovering. If you can, shower or rinse before you nurse for the first time post hard effort. Studies have shown that lactate acid can turn naturally sweet mother’s milk a bit sour, and will remain in the milk for about an hour post exercise. **Most babies do not mind the lactic acid and nurse just fine. There are no harmful effects.
You’re going to need extra sleep (laughing right?); runners require extra sleep, nursing mother-runner’s even more, but getting enough sleep with a new baby can be difficult. Try nursing laying down, get off your limbs and rest with your lil thang as much as is possible.
Remember, your body’s no. 1 priority is to maintain its milk supply. This might mean that you don’t recover from hard workouts and high mileage as fast as you would if you weren’t nursing. “With energy diverted to churning out the liquid gold, there’s less to go around for “extras” like fixing that tweaked hammie posthaste.”
ARTICLES
Running Research: Running and Nursing
Exercise and Breastfeeding
Personal Blog – Running & Nursing by Jill Will Run
Got Milk? Running and Breastfeeding
For Pregnant Marathoners, Two Endurance Tests
This Runner Mama Ran for Two at the Boston Marathon
2015 Moms’ Picks: Best Breast Pumps
Helpful tips:
1. Drain your boobs before you run – If they’re full, they’re sure to hurt.
2. Wear a comfortable sports bra – “For most nursing moms, comfortable = supportive.” Or this could mean protection from leaking.
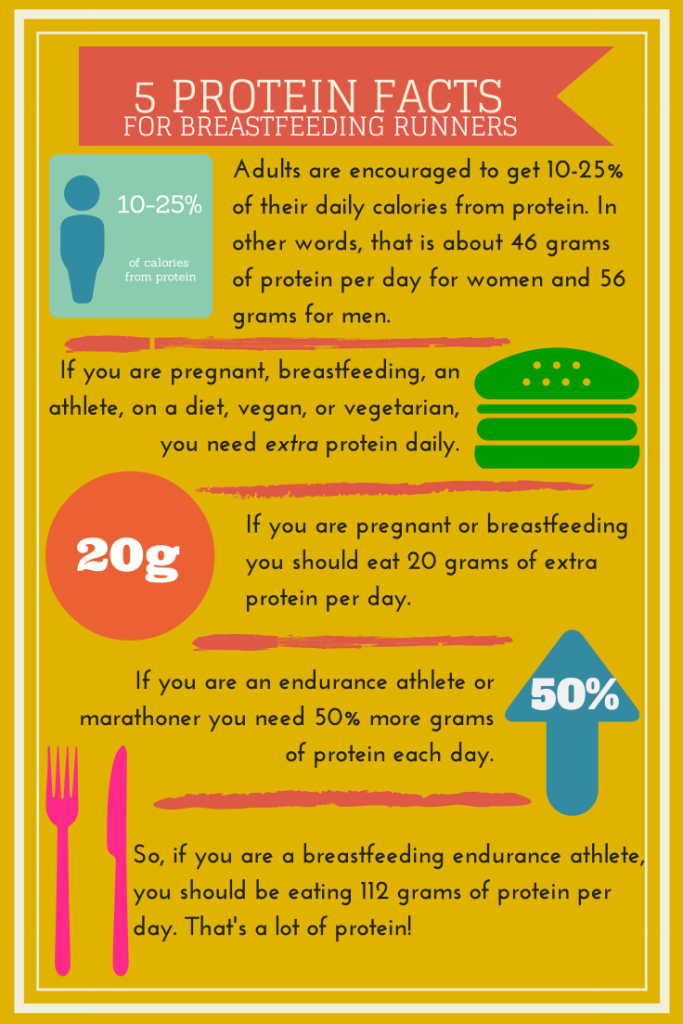
3. Eat plenty of protein – Carb-heavy diets don’t have the benefit of a lasting energy source. Breastfeeding mothers tend to require about 20 more grams of protein each day than non-nursing women, and endurance athletes need 50% more protein than non-athletes. If you’re a nursing runner – that’s a lot of protein!
4. Watch your calcium intake
5. Hydrate well